Sending a signal
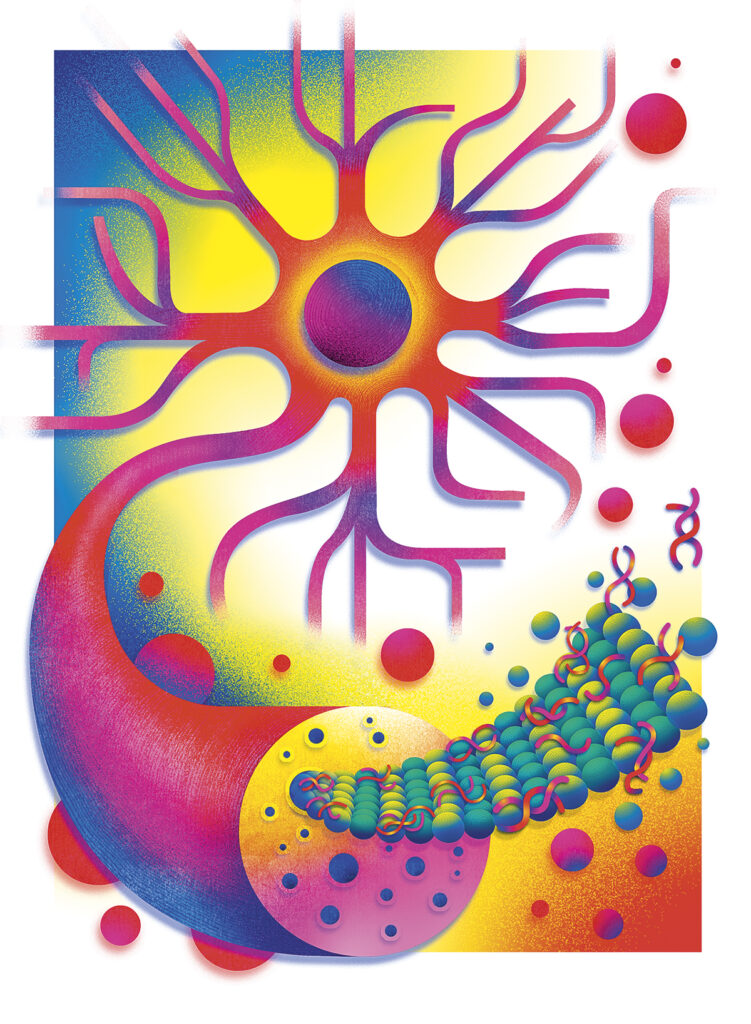
Could simple blood tests for telltale substances in the body give doctors new ways to detect and treat severe diseases like Alzheimer’s?
by Chris Quirk

Illustrations by Maria Corte
Alzheimer’s disease can present a frightening prospect, and especially for those with a family history of the illness, in large part because so little is known about it. There is no definitive diagnosis of the disease short of an autopsy, and the disease can creep up on anyone, destroying cognitive capacities and memory, and slowly robbing a person’s ability to function and to care for themselves. There is currently no cure, but as one alumna has recently discovered, there may be new developments in how the disease is flagged and managed.
Dr. Kellyann Niotis ’12 and her colleagues at the Institute for Neurodegenerative Diseases (IND) are studying several blood tests that detect key biomarkers for Alzheimer’s disease. (See “What are biomarkers?” box below.) These tests have the potential to identify people who may be at risk before symptoms start. The results, part of the IND’s Biorepository Study for Neurodegenerative Diseases, were released in April at the annual meeting of the American Academy of Neurology. This research could change the way Alzheimer’s disease is diagnosed and tracked, and open new avenues for successful treatment therapies.
According to the Alzheimer’s Association, more than 7 million people in the United States have Alzheimer’s disease, including one in nine over age 65, and the number is increasing as the nation’s population ages. For women, the lifetime risk for getting the disease is twice that of men. The Mayo Clinic says while memory loss is the primary symptom of the disease, it can also affect personality and judgment.
Niotis, who studied biology at Lafayette and graduated summa cum laude, is the director of Parkinson’s Disease and Lewy Body Prevention Research at the IND, and the founder of Preventive Neurology Practice, a private medical practice in New York City. She was a lead author on the IND study, and has dedicated her professional career to finding new paths for detecting and treating Alzheimer’s and related neurological diseases.
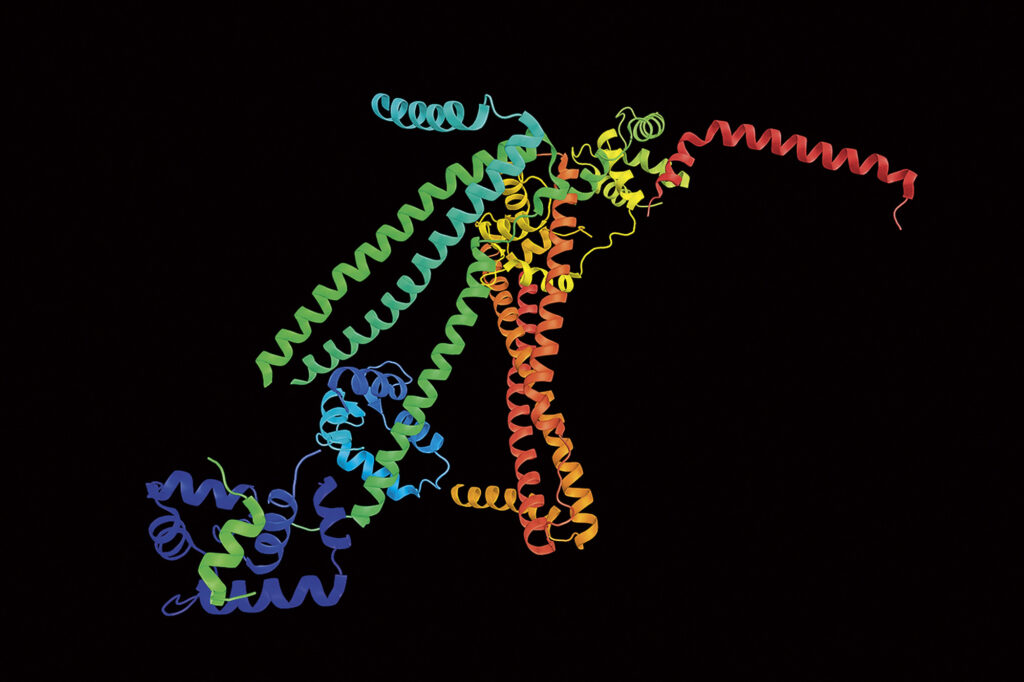
What is a biomarker?
A biomarker is a measurable biological entity of your body. It can be something common like blood pressure or cholesterol, or a substance hard to find or that appears in very small quantities, for which medical researchers often need to create a customized test to detect.
Biomarkers can give physicians specific and detailed information on what is happening with an organ or metabolic system in the body, and can help clinicians decide on and monitor the effectiveness of treatments.
In addition to biomarkers for Alzheimer’s disease and cardiovascular disease, some new and promising biomarker research into treating severe diseases is currently underway.
- A new biomarker test shows promise for detecting cancer of the pancreas at an early stage. Pancreatic cancer is typically found only after it has metastasized, and mortality rates are high. A new meta-study indicates particular proteins associated with early-stage pancreatic cancer, which could lead to more timely diagnoses.
- Another biomarker study has shown improved survival rates for estrogen receptor-positive breast cancer patients. The researchers used a biomarker that measured endocrine activity to identify the best patients for more frequent chemotherapy doses, which increased overall survival by 15%.
- Researchers are also in the early stages of research on the use of peripherin, a protein, as a biomarker for brain and nervous system damage. The presence of abnormal forms of peripherin is associated with ALS, a progressive disease of the nervous and musculature systems.
In the absence of a gold-standard determination that a patient has Alzheimer’s, doctors rely on expensive PET scans, which expose a patient to a high amount of radiation, or they use a lumbar puncture, which is invasive, to check for signs of the disease. The biomarker research study conducted at IND, however, focuses on simple blood tests, which can be performed in a doctor’s office. Similar blood tests are nearly 90% accurate in detecting Alzheimer’s disease in those with cognitive symptoms, but what is innovative about Dr. Niotis’ work is that she and her team aim to identify warning signs of the disease before symptoms start.
How do these blood tests work? They detect the amounts of p-tau 217 and amyloid beta 42 in the blood—both of which are proteins that indicate a risk for Alzheimer’s. “Based on all of the literature out there, we put together our bespoke [blood] panels of what we think were the most important and impactful, not only for Alzheimer’s disease, but related diseases like Lewy body dementia and Parkinson’s disease,” Niotis says.

Niotis says that these tests have the potential to identify people who
may be at risk for Alzheimer’s before symptoms start.

An early detection of Alzheimer’s is critical for treatment and potentially delaying the impact and progression of symptoms. In a 2024 report by CNN, Dr. Maria Carrillo, chief science officer of the Alzheimer’s Association, said that this new IND screening could change the face of Alzheimer’s care and the improvement of patient outcomes. “The p-tau 217 blood test is turning out to be the most specific for Alzheimer’s and the one with the most validity. It seems to be the front-runner,” she said. “These are absolutely transformational times.”

Reckoning risk factors
One patient whom Niotis is caring for has shown a remarkable response to a comprehensive care regimen that includes drug therapy and lifestyle changes. “Penny Ashford came to me a couple of years ago, and she was terrified because she had started to experience word-finding difficulties, which is what her father had, and he had been diagnosed with Alzheimer’s,” Niotis says. Ashford, who is in her early 60s, had high visceral adipose tissue—fat around her organs—and low muscle mass. She had a self-described sugar addiction, and Niotis says while Ashford was not diabetic, there was evidence that her body was not managing glucose properly. She had issues with cholesterol as well. “Penny was what we call a walking modifiable risk factor,” Niotis says.
When tested for Alzheimer’s biomarkers, Ashford indeed had levels of amyloid and p-tau 217 that were concerning to Niotis. “There is no established range for people who are at risk, but based on what we know from our research we could tell her values were not normal,” Niotis says. She put Ashford on a personalized prevention plan that included high-intensity cardio training to reduce the visceral adipose tissue, resistance training, reduced sugar consumption, and started her on a GLP-1 agonist, a class of drugs that includes Ozempic and Wegovy. “There’s a lot of emerging information about how these drugs may change Alzheimer’s disease pathology, specifically how they may affect p-tau pathology,” Niotis says. “So we put her on the drug, and we were very careful because there’s always a risk for worsening body composition on these drugs if you aren’t using the right diet and exercise plan.”
Ashford’s response was remarkable. She cut out sweets completely, switched to a healthier diet, exercised regularly, and lost weight. A year later, her p-tau levels had plummeted. “There was a bit of skepticism with regard to these results, questioning if we could really do something to change Alzheimer’s disease pathology,” Niotis says. “Well, for the first time we have biological evidence that we changed the pathological proteins of Alzheimer’s disease.”
A case for personalized medicine
Niotis says that biomarkers and their use in risk assessment for disease are an example of how personalized medicine can lead to better health outcomes for patients. Personalized medicine uses both pharmacological and other interventions targeted to a specific individual’s risk profile, and can provide a more nuanced understanding of health to help physicians make more effective decisions.

More than 7 million people in the
United States are living with
Alzheimer’s disease.

For example, cognitive tests may miss the beginning stages of Alzheimer’s. “It’s early on, and the patient often aces the test, but that doesn’t mean there isn’t a change in the patient’s baseline,” Niotis explains. “They may also have a very high baseline intellect, and the cognitive tests won’t pick up change.”
In the case of Ashford, it was a combination of biomarker data, lifestyle information, and other factors that prompted Niotis to take immediate preventive action for Alzheimer’s. “It has been so difficult to find modifying therapies for Alzheimer’s and neurodegenerative diseases, because what might cause the disease in one person is different than what might cause the disease in another person,” Niotis explains. “We draw things like LDL or cholesterol panels, hemoglobin A1C, or blood glucose levels in people, and sometimes we just look at those numbers and think they’re in the normal range. But if we had a brain health panel to accompany these labs, it could show that a person’s amyloid proteins are out of range for their age, and this may make us reconsider some of the other labs we’re calling ‘normal.’”
Niotis says only time will tell if they have found a viable way to monitor for Alzheimer’s progression in healthy people, but she is optimistic.
“What we really need, and what we’re doing in our next study, is to compare people who are on these multimodal, personal prevention plans longitudinally over time, and see how they do compared to normal controls, and this is underway,” Niotis says. “At that point we’ll be able to actually say, ‘yes, we delayed the onset or prevented Alzheimer’s disease,’ but it’s going to take us a little time.”